23 February 2024 (Last updated: 23 Feb 2024 10:51)
Report: Scoping visit to Addis Ababa - setting up a microsurgery training programme 5-10th Nov 2023
Rebecca Shirley, James Chan, Rinah Bheekharry
.png)
Background
Metasabia ‘Meti’ Mworku Abebe visited Stoke Mandeville Hospital as a Travelling IFESSH fellow in May to June 2022. While in the UK, she gave a presentation on her practice at the Thames Valley and Wessex Hand Surgery Conference on 25th May. She attended the IFESSH Congress at the London Excel and subsequently extended her stay to join us as a delegate on the Stoke Mandeville Microsurgery Course on 13th June. Following this course, discussions about setting up a microsurgery course in Addis Ababa began.
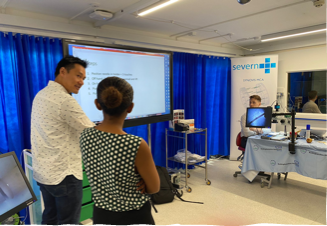
We arrived in Addis Ababa on Meti on the microsurgery course at Stoke Mandeville June 2022
.png)
COCECSA (College of Surgeons of East, Central and Southern Africa) is the largest surgical training institution in Sub-Saharan Africa, but no microsurgery training is available, and the need for microsurgery and soft tissue cover is high. St Paul’s Hospital, ABET (Addis Ababa Burn, Emergency and Trauma) Hospital, and ALERT hospitals are recognized training centres for plastic surgeons across the COSECSA countries. Many trainees from the other sub-Saharan African countries undertake their 3 years of specialist training in these hospitals. These units have all begun their journeys in microsurgery. A number of their surgeons have undertaken formal fellowship training and observerships at various reputed units, including Ganga Hospital in South India, Asan Medical Centre in South Korea, and the Chang Gung Memorial Hospital in Taiwan. They have performed free flaps for soft tissue cover this year with mixed results. Operations are largely performed with x4.5 magnification loupes e.g. donated by “Loupes around the world’ (www.loupesaroundtheworld.org). ALERT has just purchased a second-hand Zeiss operating microscope. Meti identified that there is a real need for a robust training programme.
Scoping visit from 5th to 10th November 2023
The Team
Rebecca Shirley, James Chan, and Rinah Bheekharry travelled to Addis Ababa together. They normally work as part of the hand and plastic surgery team at Stoke Mandeville Hospital, Buckinghamshire Healthcare NHS Trust. Rebecca Shirley is the Clinical Director for Plastic Surgery, James Chan is a Consultant Plastic Surgeon, and Rinah Bheekharry is an Advanced Clinical Practitioner. Since 2018, they have worked closely together tackling complex microsurgical reconstructive cases.
Rebecca Shirley
Rebecca has been a Consultant Hand and Plastic Surgeon at Stoke Mandeville Hospital for the last 7 years. She was appointed Clinical Director this year. She undertook fellowships in hand surgery at Oxford University Hospitals, microsurgery at the Marsden Hospital, London, and completed the Bruce Bailey Fellowship at Ganga Hospital, India, in 2016. Rebecca is a member of the BSSH Council.
James Chan
James has been a Consultant Hand and Plastic Surgeon at Stoke Mandeville Hospital since 2018. He undertook a one-year reconstructive microsurgery fellowship at Chang Gung Memorial hospital in Taiwan under the guidance of Fu Chan Wei. He currently serves on the Education and Training Committee of BSSH. During his training, James was awarded a DPhil (PhD) on the immunological basis of fracture healing and undertook a fellowship at Cochrane UK. He was a co-author for the BAPRAS/BOA Standards of Management of Open Fractures and is currently leading the BAPRAS Special Interest Group on diabetic foot reconstruction. His clinical practice includes reconstruction for the diabetic foot, musculoskeletal infections, and other complex wounds as well as the upper limb in tetraplegia. James has recently been appointed as Deputy Editor of JPRAS..
Together, James and Rebecca established the Stoke Mandeville Microsurgery course and have run 10 courses attracting delegates from around the UK. They also host the Stoke Mandeville Plastics webinar series which has a global reach, including many of the surgeons in Africa.
Rinah Bheekharry
Rinah is an ACP and has worked at Stoke Mandeville since 2007. She trained in Mauritius where nurses are all taught to operate during the course of their training. Therefore, she came to the UK already fully competent with suturing and managing wounds. She started as a scrub practitioner and became a team leader and theatre manager before joining the plastic surgery team in 2017. She was instrumental in setting up an excellent minor ops service. Under her leadership, this treats 150 trauma patients per month, and she has shared this experience at the BAPRAS Nurses day in 2022. More recently, she became the first free flap coordinator at Stoke Mandeville Hospital.
Key local surgeons:
AaBET (Addis Ababa Burn, Emergency and Trauma) & St. Paul’s Hospitals:
Metasebia Worku Abebe
‘Meti’ has been working as Assistant Professor of Plastic and Reconstructive Surgery at St Paul’s and AaBET Hospitals for the last four years. She is now the Head of the Plastic and Reconstructive Surgery Unit. She completed her training in Addis Ababa University and became a Fellow of COSECSA in 2018. She was awarded the International Travelling Fellowship of IFSSH in 2022 and has completed short-term fellowships in the United States through AAPS and participated in microsurgery training at the Microsurgery Training Institute at Ganga Hospital in Coimbatore, India, in 2023.
‘Bereket’ is a consultant plastic surgeon who undertook microsurgery training at Ganga Hospital in India in 2023
Dr. Abeje Brhanu – ‘Abeje’ is a consultant plastic surgeon who has completed a one year fellowship under JP Hong at the Asan Medical Centre, South Korea 2022-23
ALERT Hospital:
Dr. Abraham Gebregziabher
Recipient of the Lifetime Achievement Certificate in recognition of long years of dedicated and outstanding service as the champion of plastic and reconstructive surgeons in Ethiopia. He is the clinical director at ALERT and mentors many of the plastic surgeons in Addis Ababa and across COSECSA.
Dr. Abdurezak Ali
Dr. Abdurezak Ali is a Consultant Plastic Surgeon who has completed a one year fellowship at Chang Gung Memorial Hospital in Taiwan.

Day 1 after the teaching session with consultants (Dr. Rahel Kassa, Dr.Bereket The team on arrival in Addis Ababa Atnafu, Dr. Martha Fikremariam, Dr. Metasebia Worku-front row) and trainees (Dr. Addisalem, Dr. Misha, Dr. Bethelhem, Dr. Getnet, Dr. Tewabech, Dr. Mamush)
The Itinerary
Day 1
The team arrived at Bole International Airport on Sunday morning and were received by Meti who drove us straight to a ceremonial coffee, breakfast and then onto a tour of AaBET hospital, where the acute trauma cases are admitted. We looked around the 20 bedded burns unit and observed the nurses doing dressing changes. We saw the kitchen where nutritional food was prepared including the high protein “Bombay cocktail” containing eggs and bananas given to burns patients.

We also saw a number of trauma cases from industrial injuries and the following examples provide a glimpse of the situation.
Patient 1: 20 year old man sustained a Gustillo 3b injury to the left tibia whilst working with a grain mixer 6 weeks ago. A CT angiogram had already performed in a different hospital as part of the work up. An ALT flap and uniplanar ex-fix was attempted 3 weeks ago. Unfortunately the flap became ischaemic at day 2 and necrosed. Later that day, we were able to join the team in theatre for the debridement of the wound. We learnt that a major amputation is major issue in Ethiopia where there is no access to prosthetic support. Furthermore, culturally, patients are extremely loath to amputations and would prefer to allow the wounds to continue to fester indefinitely.
Patient 2: A middle-aged healthcare professional with an old open tibial fracture that had been reduced and stabilised with an ex-fix 7 weeks ago. There was 30 cm of exposed necrotic tibia with extensive periosteal stripping. This was not a reconstruct able defect and a below knee amputated was recommended.
Patient 3: Lady in her 40s who was cleaning a cement mixer that was accidentally switched on, sustained a right humeral fracture, a visceral injury requiring a defunctioning colostomy and a multiplanar circumferential degloving of her left ankle and hind foot as well significant bone loss of the os calcis. We agreed that reconstruction would lead to a poor short-lasting outcome and recommended a below knee amputation.
Patient 4: A young woman with a flexor sheath infection with her finger buried into her chest.
Patient 5: An older woman with an exposed fibula plate for an united fracture from 2 months ago. We advised removal of the plate, wound debridement and dressings/peroneus brevis flap as a simple solution to getting the wound healed.
We returned to AaBET hospital later in the day to help with the debridement of the ALT flap in Patient 1. The flap was necrotic and sloughy. There was a 12 cm section of exposed tibia distal to the fracture site with periosteal stripping. The bone was still viable although there was a non-union with a 1.5cm bone gap. The team planned an orthoplastic procedure to address the non-union and reconstruct the soft tissue defect with a second free flap for Tuesday (Day 3).
Day 2
We travelled to St Paul’s Hospital to meet the Plastic Surgery Department and deliver an interactive educational session from 10 am to 1 pm. We were welcomed by the Head of Surgery, Professor Engiga Abebe, who was a transplant surgeon himself and very keen to support the development of the microsurgical service. We were able to meet the team of 12 consultants and trainees. We introduced ourselves and explained about the work we do in the UK, how we developed our extremity reconstructive microsurgical service and how the free flap pathway currently works in our unit. Both teams sharing their personal experiences of microsurgery and a good discussion was generated around the talks, including the importance of teamwork (including anaesthetists, AHPs), human factors, patient selection, work horse flaps and post-operative monitoring. We also learnt about the possibilities and limitations of the setting of St. Paul’s and the types of patients the local surgeons felt would benefit from such a service (largely trauma and oncological).
In the afternoon, we returned to AaBET Trauma hospital to see more patients including two teenage sisters. They had sustained high voltage electrical injuries in one of the surrounding villages when their sickles, used for cutting barley, came into contact with a low hanging high voltage wire. The older sister had been trying to save the other. They both presented with similar injuries: large soft tissue defects over their right dominant wrists with exposed distal radius and ulnar to a routine out-patient appointment many weeks after the neglected injuries. The hands were unstable but viable, vascularised by narrow skin bridges on the ulnar artery in one case and on the radial artery in another. There are over 90 languages spoken in Ethiopia and both girls spoke Oromifa, a dialect from their rural village but no Amharic, the official language in Addis Ababa. An older sister was able to translate. Amputation was also offered and the patients and their family were adamant that they would not consent to this. They were insistent for any reconstructive effort to provide an assist hand. The team concluded that for the younger sister, the wound could be debrided with minimal bone resection and the soft tissue defect could be covered with an abdominal or groin flap. However, the older sister would require a free fibula flap as there was no bony stability and a huge segmental loss of both radius and ulnar. The patients and their family (mother and sisters) were fully consented by the local surgeons including what the surgery would entail and the benefits and risks.
Day 3
We joined the local team including two consultants, Meti and Bereket, in theatre to perform a second ALT flap in patient 1. An orthoplastic approach was adopted. The orthopaedic surgeons debrided the bony non union and readjusted the uniplanar frame to a multiplanar configuration to achieve good bony contact with compression. A second ALT was well executed and a decision was to use the proximal anterior tibial vessels again as it exhibited good flow although there was a significant size mis-match. An end to side onto another vessel would have been riskier with the lack of good magnification with a microscope. The procedure was technically well executed and the flap was well perfused at the end of the operation. Unfortunately, it appeared that there was arterial insufficiency overnight and by the time of take back the following morning, the flap was unsalvageable. This prompted further discussions about the peri-operative management including flap monitoring and prompt recognition +/- take back post-op. The plan now is to provide soft tissue coverage with a regional muscle flap which the local team will perform in the subsequent days.
Day 4
The teenager with flail right hand was taken into theatre for wound excision and a free osteocutaneous fibula flap reconstruction. Meti, Bereket and Abeje all operated with us jointly. This was a complex case requiring segmental excision of the distal radius and ulnar and fixation of the fibula to the distal radius and wrist. A long saphenous vein graft was required. The case went well and through regular WhatsApp communication, we are being kept abreast of progress and the patient is currently undergoing rehabilitation.
Day 5
We visited ALERT Hospital where we were received by Dr Abraham, one of the most respected senior plastic surgeons in Ethiopia and COSECSA. Over the past few years, he has started developing the microsurgery programme at ALERT, making connections internationally and encouraged the young dynamic colleagues to go on fellowships and observerships, reminiscent of how the microsurgery services developed at Ganga Hospital and Chang Gung Memorial Hospital. He plans to run a training programme and showed us around the hospital including the clinical, research and teaching facilities. Their training facilities are excellent, including a large, dedicated room for simulation training which would be ideal for microsurgery training with bench space for training microscopes. There is accommodation on site for delegates and facilitators/instructors. We were also shown around ITU and theatres including the reputed Kids OR where there is a second hand Zeiss operating microscope and where he foresees the microsurgery cases will be regularly undertaken. We met some of his consultant colleagues and trainees including international ones from Kenya and Tanzania.
Donation of Mesher from the UK:

A Brennan Mesher for skin grafting which was formerly used at Stoke Mandeville Hospital was donated to AaBET Hospital. This will enable the hospital to treat burns over 20% that previously had to be referred to another hospital. The Mesher has no disposable parts so will not incur any addition cost. The Mesher was put into use immediately.
Impression:
The vision of the local teams in Addis Ababa led by Meti and supported by Dr Abraham is that Addis will become a designated centre for microsurgery training for the COSECSA countries. The microscopes would be used by local trainees throughout the year and courses lasting three days would be offered to COSECSA members initially twice a year.
At ALERT, AaBET and St. Paul’s Hospitals in Addis Ababa, there is a critical mass of surgeons who perform microsurgery. They feel that with training microscopes in place, the combined team are ready to set up their course.
These units have the right leadership and people, the basic infrastructure and demand to continue developing a microsurgical service safely. We have been mightily impressed by their determination, resiliency, knowledge and skills. They have identified the need for a robust training programme, including simulation using training microscopes. This will not only help the local population in Addis Ababa but also impact the rest of Ethiopia and COSECSA countries as they serve as two of the major plastic surgical training centres in the sub-Saharan Africa. We are well placed to facilitate this phase of development.



Visit to Alert hospital: The newly donated operating microscope, with Dr Abraham in the area designated as the microsurgery training lab, the team in theatre with Dr Abraham and in theatre with his consultant colleagues. – Dr. Endale Kefale, Dr. Meklit Birhane, Dr. Hillina Legesse.
Proposed plan designed by the local surgeons and the scoping team:
- Virtual educational support:
- Webinars with Raja Sabapathy, Fu Chan Wei et al to share their experiences of setting up microsurgical centres from the beginning.
- Joint case conferences every 4 months with AaBET. St. Paul’s and ALERT to discuss potential cases and share experiences
- Webinars with African peers for them to share the pathologies that they encounter e.g. leprosy reconstruction, traumatic injury patterns that are less common in developed nations. We will invite experts from the hand and plastic surgery communities in the UK and other developed nations.
- Complete a mini-documentary using videos and photographs we took on the trip to inform about the local surgeons’ experiences of hand and reconstructive plastic surgery in Ethiopia and the limitations they face.
- Raise funds for equipment including training microscopes, microsurgery kit, sutures, silicone vessels, screens.
- Rinah will liaise with their Theatre Manager and Lead Scrub Nurse to organise microsurgical specific sets and educate about maintenance of instruments. She will also consult about setting up a running of the free flap pathway including the perioperative logistics and post-op flap monitoring.
- Regular 12 monthly visits (7-10 days) including a wider team e.g. anaesthetist – facilitate microsurgery course, observe/participate in selected cases.
- Encourage publications of local experience – JC will help design cohort studies with view to publish in peer-reviewed journals.
View Other News Articles